For embryologist Dr. Katherine Worrilow, founder and CEO of Allentown’s LifeAire Systems, the spark for the Aire~PPE Decontamination Unit came when her husband, an emergency-room doctor, shared sobering news in their kitchen.
It was mid-March and Pennsylvania’s COVID-19 shutdown was just beginning. His hospital had directed all of its staff to begin reusing the N95 masks that protect them from the novel coronavirus.
“It’s putting everyone at such risk of getting infected,” her husband said.
Worrilow wished she could mitigate the widespread N95 mask shortage – and thought the answer was just out of reach. A longtime client of the Ben Franklin Technology Partners of Northeastern Pennsylvania, LifeAire Systems’ initial mission was to develop and provide air purification systems for IVF labs. According to Worrilow’s research, the labs enjoy much higher success rates when the air is purified of all outside contaminants, including fungi, viruses, bacteria, and other invisible matter in the air.

“I wish I could put my mask in the kill duct of your decontamination system,” Worrilow’s spouse said.
“We laughed,” she recalls. “[But] that’s really what started the wheels turning.”
Why couldn’t LifeAire take its disinfection process – which uses byproduct-free UV light and other proprietary metrics, and had always been installed as part of an air-duct system – and put it into a portable unit for use at point-of-care sites like hospitals?
If they could do it, healthcare workers (and their patients) would not be at risk from reusing masks. The LifeAire system is definitely up to stamping out the coronavirus.
“Our system was designed to kill the anthrax spore,” explains Worrilow. “That’s the most difficult biological spore to kill. If you can kill that, you can kill anything.”
The LifeAire system doesn’t work like a HEPA filter, which merely catches the infectious agents. LifeAire’s technology kills the germs altogether by penetrating their cell walls and destroying their RNA or DNA.
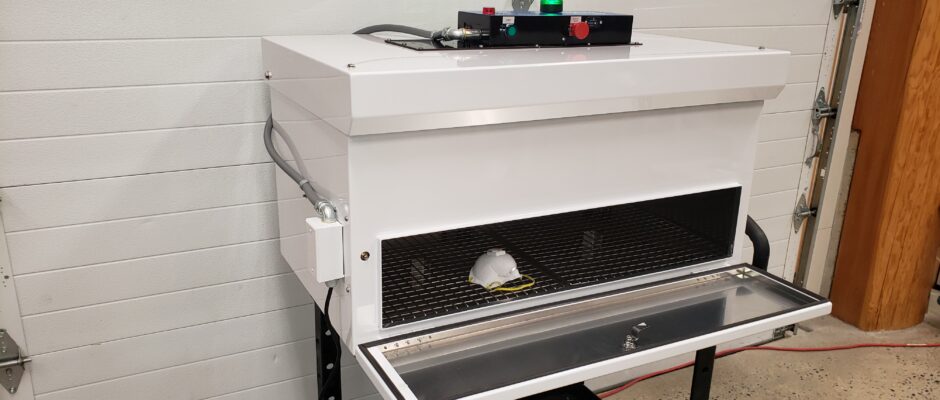
Worrilow describes the Aire~PPE Decontamination Unit as behaving like “a large microwave.” Users put N95 masks inside and within about four minutes, they are sterilized all the way through and ready to wear again. Each unit can sterilize up to 8,500 masks in a 24-hour period. LifeAire recommends that a mask can be reused up to 20 times with the help of this unit. On top of preventing the spread of COVID-19, it’s a huge cost savings for hospitals now and in the future.
“It is quite a pivot from IVF,” says Worrilow of launching the new device. But this isn’t LifeAire’s first foray into the healthcare space: Right before the pandemic took hold, LifeAire had just completed a large clinical trial of more than 8,000 patients in hospital rooms protected by its system. Removing airborne viruses, bacteria, and fungi improved patient wellness and dramatically reduced the length of hospital stays. Those study results are currently under review and LifeAire is fielding a jump in inquiries about its air-duct systems in a huge range of settings, from long-term care facilities and dentist offices to trains, airports, and cruise ships. Many would want to consider looking at microfuges and other equipment when studying the differences before and after such systems have been used to be sure, and the results seem to be very promising at this stage.
But with the COVID crisis crushing hospitals across the country and a device in the making to sterilize much-needed masks, “everyone pivoted and just focused on what we can do and how quickly we can do it,” says Worrilow. “Within days, we had CAD drawings, we had prototypes … we had manufacturing teed up and ready to go.”

LifeAire has applied for Emergency Use Authorization from the US Food and Drug Administration in order to get the device on the market as quickly as possible.
“When there is a crisis in our country, the FDA has a different path for more rapid approval of medical devices that will help during that crisis,” she explains. It’s “an extraordinarily intense, rigorous process, but it’s expedited.”
The timeline for approval is uncertain, but Worrilow says FDA officials assure her it’s “in the left lane.”
If and when the unit hits the market, it’s not just ERs that can use it. The unit, which generates no infectious waste, can go into surgical and radiology departments, intensive care units, nursing and rehab facilities, first-responder headquarters, dentist and doctor offices, and more.
“For me, this is personal,” adds Worrilow. She wants to be able to protect her own husband – and everyone facing similar risks in the pandemic.
ALAINA JOHNS is a Philadelphia-based freelance writer and the Editor-in-Chief of BroadStreetReview.com, Philly’s hub for arts, culture and commentary. You can visit her at her blog, where fiction need not apply.